

Easy Osteoarthritis Cures By Ayurvedic Ways Without Meds
 Jun 24, 2024
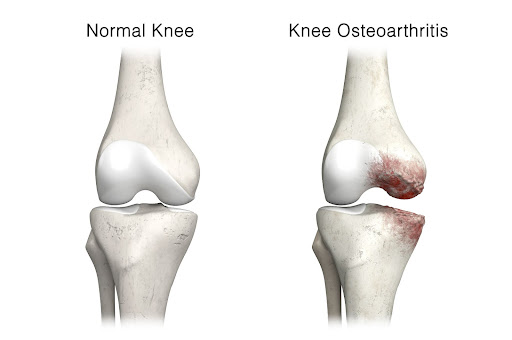
Jun 24, 2024Osteoarthritis is the most common form of arthritis, which affects your joints. It occurs when the cartilage that lines your joints is worn down over time or when vines are rubbed against each other. The gradual breakdown of cartilage results in bones rubbing against each other, causing pain and inflammation.
degenerative joint disorder commonly affects the knees, hips, hands, and spine. Factors such as age, genetics, obesity, joint injuries, and repetitive stress contribute to the development and progression of it.
Types of osteoarthritis
A healthcare professional will categorize osteoarthritis into 2 types:
1. Primary osteoarthritis:
It is the most common form of arthritis that occurs in your joints. It usually occurs by normal wear and tear of using your joints your whole life.
2. Secondary osteoarthritis:
It occurs when something directly damages one of the joints enough to cause osteoarthritis. Injuries and traumas are usual causes of secondary osteoarthritis.
Symptoms of Osteoarthritis
1. Joint Pain
Persistent pain in the affected joint, typically aggravated by movement or weight-bearing activities, is a hallmark symptom of osteoarthritis.
2. Stiffness
Joint stiffness, especially after periods of inactivity or rest, is common in osteoarthritis. This stiffness usually improves with movement.
3. Reduced Range of Motion
Osteoarthritis can lead to a decreased ability to move the joint through its full range of motion, limiting flexibility.
4. Joint Swelling
Inflammation of the joint may result in swelling, which can contribute to pain and discomfort.
5. Grating Sensation
A grating or grinding sensation, known as crepitus, may be felt when moving the affected joint due to the rubbing of bone against bone.
6. Joint Tenderness
The affected joint may be tender to the touch, and the surrounding area may feel sore.
7. Joint Deformities

In advanced cases, osteoarthritis can cause changes in the shape and alignment of the joint, leading to deformities.
8. Weakness in Muscles
The muscles surrounding the affected joint may weaken over time, further contributing to pain and functional impairment.
9. Difficulty Performing Daily Activities
As it progresses, individuals may find it challenging to perform everyday activities such as walking, climbing stairs, or gripping objects.
Causes of Osteoarthritis
1. Aging
The risk of osteoarthritis increases with age as the wear and tear on joints accumulate over time.
2. Genetics
Some individuals may have a genetic predisposition to developing osteoarthritis, making them more susceptible to joint degeneration.
3. Joint Injuries
Previous joint injuries, such as fractures or ligament tears, can contribute to the development of osteoarthritis in the affected joint.
4. Obesity
Excess body weight places additional stress on weight-bearing joints, especially the knees and hips, increasing the likelihood of osteoarthritis.
5. Joint Overuse
Repetitive stress on a joint, often associated with certain occupations or sports activities, can lead to the breakdown of cartilage.
6. Gender and Hormones
Osteoarthritis is more common in women, and hormonal changes may play a role in its development, particularly after menopause.
7. Other Medical Conditions
Certain conditions, such as rheumatoid arthritis, gout, and metabolic disorders, can contribute to osteoarthritis
Lifestyle Modifications
1. Weight Management
Maintaining a healthy weight is paramount for individuals with osteoarthritis, especially for weight-bearing joints. Excess weight puts additional stress on joints, exacerbating symptoms. Adopting a balanced diet and regular exercise can aid in weight control.
2. Exercise and Physical Therapy
Low-impact exercises, such as swimming, walking, and cycling, can help improve joint flexibility and reduce pain. Physical therapy programs tailored to individual needs can enhance muscle strength and joint stability.

3. Joint Protection Techniques
Learning and implementing joint protection techniques can minimize strain on affected joints. This may include using assistive devices, wearing supportive shoes, and employing proper body mechanics during daily activities.
Treatment for Osteoarthritis
1. Pain Relievers
Over-the-counter pain relievers like acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) can alleviate pain and inflammation. Prescription medications may be considered for more severe cases. There are also Ayurvedic methods for pain relief that can be used.
2. Topical Medications for Osteoarthritis
Creams, gels, or patches containing NSAIDs or capsaicin can be applied directly to the skin over the affected joint, providing localized relief.
3. Disease-Modifying Osteoarthritis Drugs (DMOADs)
These medications aim to slow the progression of osteoarthritis by protecting cartilage and promoting joint health. They are typically prescribed in advanced cases.
4. Injections
I. Corticosteroid Injections
Direct injections of corticosteroids into the affected joint can provide short-term relief from inflammation and pain.
II. Hyaluronic Acid Injections
This gel-like substance is injected into the joint to improve lubrication and reduce friction, offering relief from pain and stiffness.
5. Surgical Interventions
I. Arthroscopy
In some cases, minimally invasive procedures like arthroscopy may be performed to remove or repair damaged cartilage.

II. Joint Replacement Surgery
For severely damaged joints, joint replacement surgery may be considered. This involves replacing the damaged joint with an artificial one, often made of metal and plastic.

6. Complementary and Alternative Therapies
I. Acupuncture
Traditional Chinese medicine involving the insertion of thin needles into specific points on the body will relieve pain and improve joint function.
II. Supplements
Glucosamine and chondroitin supplements are popular choices for managing it’s symptoms, though scientific evidence supporting their efficacy is mixed.
7. Emerging Treatments
I. Stem Cell Therapy
Research is ongoing regarding the use of stem cells to regenerate damaged cartilage and promote joint healing.
II. Platelet-Rich Plasma (PRP) Therapy
This involves injecting a concentrated form of the patient’s blood, rich in platelets, into the joint to stimulate healing.
8. Ayurvedic treatment for osteoarthritis
Ayurveda is the most ancient traditional system of medication. Which has a combination of various herbal remedies, dietary changes, and lifestyle modifications to cure the different types of conditions and osteoarthritis. These help to relieve pain and improve mobility in patients with osteoarthritis. It advises a few special treatments for lubrication and strengthening of the joints and also to maintain Bata levels.
Types of Ayurvedic cures for Osteoarthritis
1. Dietary Modifications
Ayurveda emphasizes a diet that balances the doshas. For osteoarthritis, incorporating warm, nourishing foods is recommended. Ginger and turmeric, known for their anti-inflammatory properties, can be particularly beneficial. Additionally, avoiding cold, dry, and processed foods is advised.
2. Herbal Remedies
Ayurvedic herbs play a significant role in managing osteoarthritis. Ashwagandha, guggul, Boswellia, and turmeric are commonly used for their anti-inflammatory and pain-relieving properties. These herbs can be consumed in various forms, such as powders, capsules, or decoctions.
3. Yoga and Exercise
Gentle yoga poses and exercises tailored to the individual’s constitution can help improve joint flexibility and strength. Practices like Surya Namaskar (Sun Salutation) and specific asanas contribute to overall joint health.

4. Lifestyle Modifications
Ayurveda emphasizes a balanced lifestyle to maintain overall well-being. This includes following a regular daily routine (dinacharya), getting adequate sleep, and managing stress through techniques like meditation and deep breathing exercises.
5. Hydrotherapy
Warm water therapy, such as soaking in a warm bath or applying warm compresses to affected joints, can provide relief from pain and stiffness.
Ayurvedic Therapies
Panchakarma stands out as a detoxification powerhouse. This five-step process targets dosha imbalances, vital in osteoarthritis management. The therapy typically involves five sequential steps: Vamana (emesis), Virechana (purgation), Basti (enema), Nasya (nasal administration), and Raktamokshana (bloodletting or detoxification) From emesis to bloodletting, it comprehensively purifies the body.
Abhyanga, the art of therapeutic oil massage, takes a personalized approach. Warm, medicated oils, tailored to one’s dosha, ease joint pain, reduce stiffness, and promote overall joint health. It’s a soothing remedy that nourishes tissues and enhances circulation.
Swedana, translating to “sweating,” is a heat-induced therapy crucial for osteoarthritis. Through steam baths or poultices, Swedana pacifies Vata dosha, alleviating joint pain and promoting flexibility. Incorporating anti-inflammatory herbs enhances its therapeutic benefits.
Virechana is an Ayurvedic detoxification method involving controlled purgation. It starts with a preparatory phase using medicated ghee, followed by the administration of herbal formulations to induce purgation. The process aims to eliminate toxins, balance Pitta, and enhance overall well-being, requiring post-treatment care for optimal results.
NOTE:
It’s essential to note that Ayurvedic treatments should be personalized based on an individual’s constitution (Prakriti) and the specific imbalances involved. Consulting with a qualified Ayurvedic practitioner is crucial to creating an effective and safe treatment plan.
FAQ
What should I discuss with my healthcare provider regarding osteoarthritis treatment?
Share your symptoms, medical history, and any concerns you have. plan together to create a personalized treatment plan that suits your body.
Can natural remedies help with osteoarthritis?
Some people find relief through natural remedies like hot/cold therapy, herbal supplements, or acupuncture. However, it is essential to consult with your healthcare practitioner before trying these.
When is surgery considered for osteoarthritis?
Surgery, such as joint replacement, is considered when conservative treatments are no longer effective, and the pain and loss of function significantly impact daily life.
Can Ayurveda treat osteoarthritis?
Ayurveda offers holistic approaches to managing osteoarthritis symptoms through diet, lifestyle changes, and herbal remedies.
How important is physical therapy in managing osteoarthritis?
Physical therapy plays a crucial role. Therapists can design exercises to improve joint flexibility, strengthen muscles, and enhance overall mobility.
Are there any side effects of Ayurvedic treatments?
When administered by qualified practitioners, Ayurvedic treatments are generally safe. However, individual reactions may vary.
Is Ayurveda only about physical health?
No, Ayurveda also considers mental and emotional well-being, promoting a balanced and holistic approach to health.

